New arthritis treatment in dogs!
There is now a new treatment for arthritis in dogs! Degenerative joint disease is very common in older animals and can severely affect their
There is now a new treatment for arthritis in dogs! Degenerative joint disease is very common in older animals and can severely affect their
An update on Pet Travel to the EU and Northern Ireland. Pet travel to the EU now that the transition period has ended.
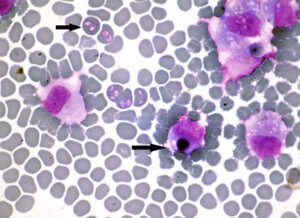
It has been in the news that some dogs in Essex have been infected with Babesia Canis and become very ill. This is news because
Rules on taking your pet abroad to most EU has become more far more relaxed. Taking your pet with you on holiday is now far
It was a cold winters day and Barley was snuggled up in his basket when he heard his dad return home from work. ‘Great!’ he
Puppies are about the most adorable organisms on the entire planet, but the fantasy of snuggling in a warm pile of little doglets can be
Having just picked up your new puppy, you are excited about your puppy and want to do the best for it. Now where to go
Chocolate poisoning in dogs. Dogs are susceptible to chocolate poisoning. This is because they are more sensitive to the poisonous ingredient (theobromide), they are
What is a Histiocytoma? These are usually angry looking, raised, hairless masses found on the skin of young dogs. The most common areas are on the
Dental care is a discipline in veterinary medicine that was often not performed as well as we might have liked. There are many reasons for